By Charles Leach, M.D.
(c) Connecticut Explored Inc. Feb/Mar/Apr 2004
Subscribe/Buy the Issue!
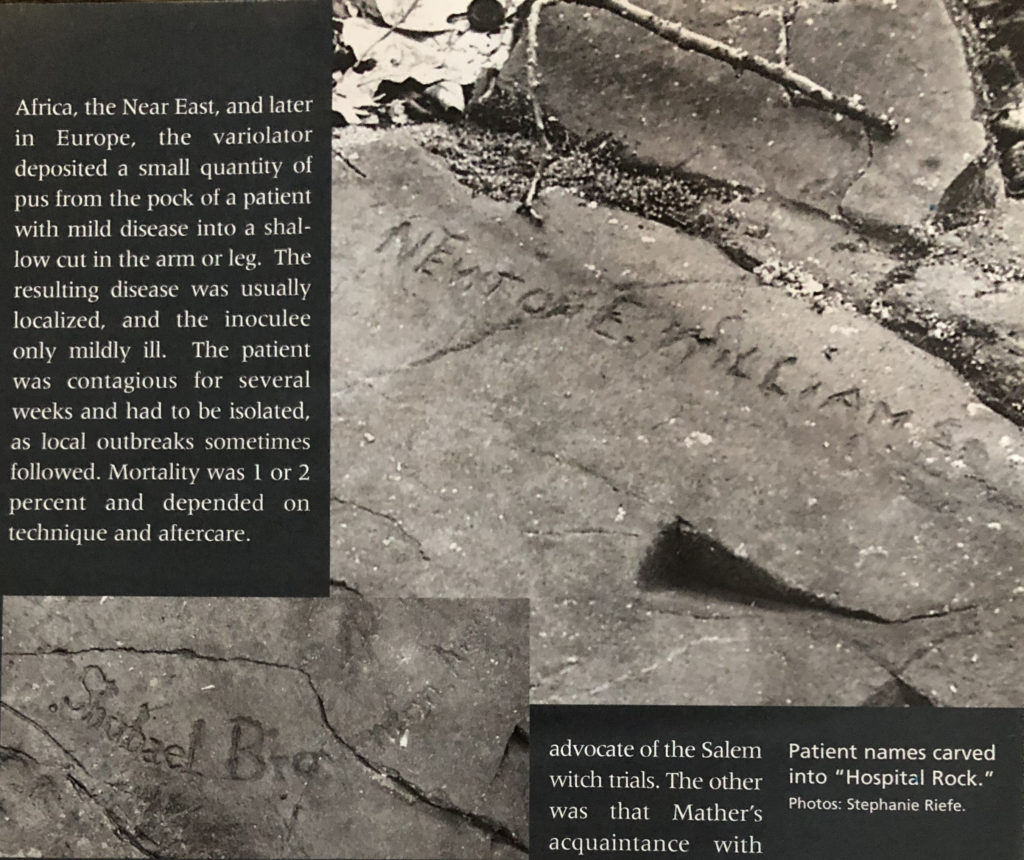
Hidden deep in the second-growth hardwood forest of Rattlesnake Mountain is an inconspicuous flat ledge of traprock. On it are carved 66 names of long-ago Farmington residents. This is Farmington ‘s “Hospital Rock,” and it marks the site of Eli Todd and Theodore Wadsworth’s smallpox inoculation hospital of the 1790s. It is a reminder of the terrible epidemics of another day, and of the efforts of local physicians to halt their spread.
In colonial New England villages like Farmington smallpox epidemics were infrequent, but the inhabitants were more susceptible than city dwellers when outbreaks did occur. A rural population would become immune as the result of infection, and another outbreak would not occur until five to 20 years later, when a critical mass of susceptibles was again present. The larger towns and cities, on the other hand, experienced small outbreaks of the disease with such frequency that it was almost endemic. Their populations carried a high level of immunity, and were protected for life after a childhood infection. The grim folk wisdom was that one’s child was not one’s own until it had survived smallpox. Most children did in fact survive, and their mortality was lower than that of adults, for whom the death rate was 20 to 30 percent.
The Virus and the Disease
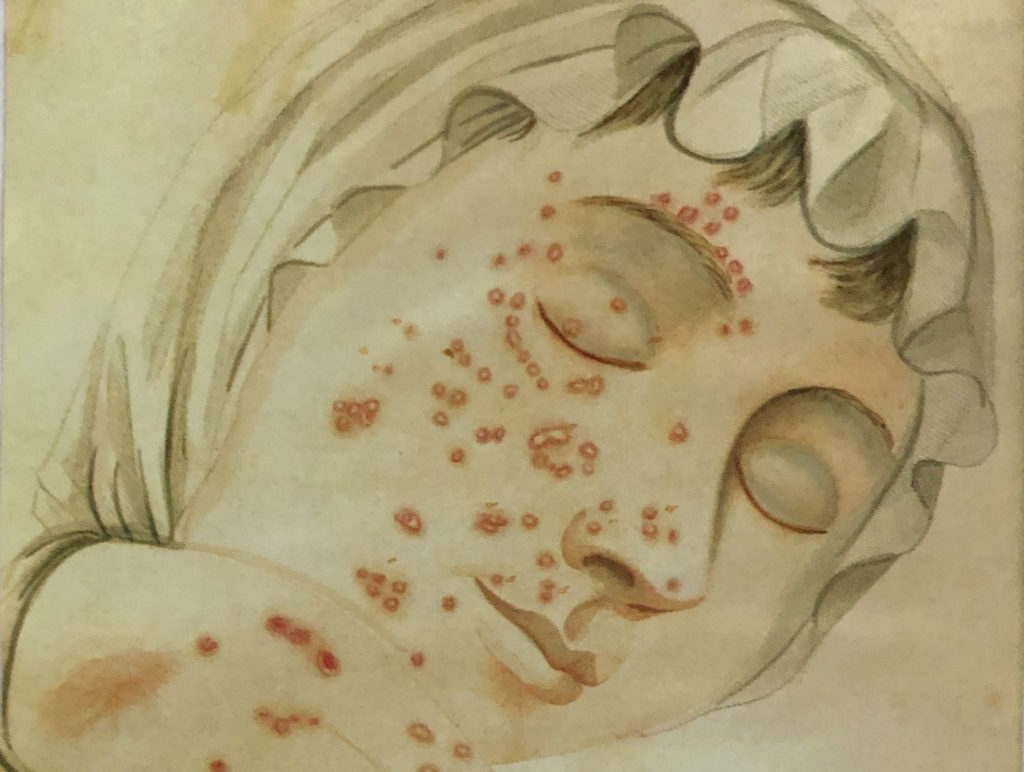
Illustration of small pox from Dr. John D. Fisher’s “Description of the Distinct, Confluent, and Inoculated Small Pox, Varioloid Disease, Cox Pox, and Chicken Pox,” 1836
The smallpox (“variola”) virus consists only of two twisted strands of DNA. It is smaller than the smallest bacteria, and unaffected by antibiotics. It is a member of the Orthopox virus group, which includes several animal pox viruses. Humans have been its only reservoir; the virus was neither carried by insects nor did it affect animals. For this reason quarantine was effective as a preventive measure if instituted in time. However, because of its long incubation period, a victim could transmit the virus before its presence was recognized, especially since it survived for many days on the bedding and clothes of victims. These “fomites” have been an important means of spread. There are several strains of the virus, and consequently the severity of the illness has varied considerably geographically and over time.
John Adams called smallpox “The King of Terrors,” and Thomas McCaulay referred to it as “The most terrible of the ministers of death.” Gurdon Buck’s 1858 medical textbook referred to it as “the most loathsome and fatal disease known to man.” The disease was usually acquired by inhalation of respiratory droplets. After roughly 12 days it would manifest with high fever, headache, backache and nausea. The characteristic rash developed over two weeks; small, deep nodules evolved into pustules in the thickened and inflamed skin. These might be few in number, or they might cover much of the body. The lesions would then dry and form scabs over a two- to three-week period. The pustules might also hemorrhage and merge into a single, malodorous mass. Rotting sheets of skin might be shed, and stick to bedclothes. Respiratory tract and eyes could be involved, and blindness could result. In severe cases, the victim was physically dehumanized and unrecognizable by loved ones. Transmission can occur until the scabs are shed; scab-laden bedding and clothing is infectious for days or weeks. The end result for survivors was disfiguring and often extensive scarring, but lifelong immunity.
Smallpox arrived in the New World with the Spanish conquistadors in Central America in 1519. A great epidemic in London in 1628 was exported to Massachusetts , where the disease caused havoc from 1628 to 1631. The first terrible epidemic among New England Indians wiped out more than 90 percent of the tribes along the coast and in the Connecticut Valley in 1633 and 1634. Subsequent outbreaks occurred in 1638, 1648-49, 1660, 1666, 1677-78 (the worst), 1689-90, and 1702-03. Finally, during a terrible epidemic in Boston in 1721, immunization was employed for the first time in America .
Variolation: “Taking the Pox by Engrafting”
Protection from smallpox could be achieved by “variolation”-voluntarily receiving a small inoculum and sustaining localized mild disease. This had been done in China by inhaling the dried scabs. In Africa, the Near East and later in Europe , the variolator deposited a small quantity of pus from the pock of a patient with mild disease into a shallow cut in the arm or leg. The resulting disease was usually localized, and the inoculee only mildly ill. The patient was contagious for several weeks and had to be isolated, as local outbreaks sometimes followed. Mortality was 1 or 2 percent, and depended on technique and aftercare.
In 1721, thousands were dying of the contagion in Boston . The Puritan divine and medical scientist Cotton Mather convinced physician Zabdiel Boylston to join him in variolating Bostonians. Boylston was severely criticized by his colleagues, and Mather himself was threatened and vilified, and his home was firebombed. Their work continued however. The results of immunization were carefully recorded, and its success was documented through one of the earliest applications of the scientific method to medicine. Mather and Boylston found that protection among 247 inoculees was virtually 100 percent. Thereafter, variolation was accepted and used in the American colonies to one degree or another. There were two great ironies in the story: one was that Mather, spanning from medieval to modern thought, was both a medical innovator and an advocate of the Salem witch trials. The other was that Mather’s acquaintance with variolation derived not only from English examples but also from his slave, Onesimus, who told him of its use in Africa .
Further major outbreaks in New England were documented in 1730-31, 1735-40, 1750-52, 1760-61, 1764, and 1772. The Revolutionary War years brought repeated outbreaks, especially among the troops. It was in this setting that Eli Todd, Theodore Wadsworth, and their contemporaries initiated the smallpox hospitals of the 1790s.
Smallpox Immunization in the 1790s
Although it had been more than a decade since the last great smallpox epidemic in America (1774-1782), for many reasons, the early 1790s was the right time for enlightened practitioners to offer immunization to their communities. Smallpox immunization in the colonies had followed a pattern of years of neglect interspersed with epidemics, which triggered urgent variolation programs. When the disease was not stalking a community, there was little enthusiasm for undergoing the risk and discomfort of “taking the pox by engrafting.” In addition to the 1 or 2 percent mortality rate, the live variola virus inoculum could spread to the community. For this reason variolation was outlawed in New England in 1761, but again permitted in 1777. In New York and the middle colonies it was more freely practiced, and many Yankees journeyed there to “receive the pox.” From time to time, local Connecticut governments prohibited the practice. Town selectmen always had the say as to when and where inoculation could be done and by whom. One Connecticut practitioner was permitted to variolate, but made to promise that he would pay a fine of 40 shillings for every case that occurred secondarily in the town. Another was fined 60 dollars for doing the procedure without permission.
The English inoculator Robert Sutton introduced safer preparation and technique in the 1760s, and the advantages of the “Suttonian Method” were well known in the colonies. In consequence, more physicians offered inoculation, and more patients accepted it. The need for isolation was better recognized and implemented. The beginnings of more sensible and kindlier treatment of the disease itself were on the horizon. Patients were no longer starved before inoculation, and many had begun to doubt the efficacy and safety of vomiting, sweats, purges, mercurials (toxic mercury salts such as calomel), and bleeding which had previously weakened both inoculees and those who “took the pox in the natural way.”
In the early 1790s roads were still very poor and often impassible, but the needs of commerce required improvements. In consequence, the era of turnpike-building began in 1792. Since troop movements during the French and Indian War had brought smallpox to Farmington in 1760, and probably during the Revolution, residents knew that contagion would increase with better highways and increased travel. Socioeconomic factors were also at work, and the earliest signs of the industrial revolution were evident. The famous Slater cotton mills began operations in 1790 in Rhode Island , and were soon emulated in Connecticut . Smallpox-susceptible farm girls and children were packed into unsanitary workplaces and habitations. And so greater social organization gave impetus to preventive efforts. Physicians had begun to form state and local medical societies- Hartford ‘s was founded in 1792-which led to greater exchange of information and awareness of new therapies, preventive and otherwise. Treatment methods were debated and improved. Often highly motivated toward the public good, the physician-variolators were also leaders of the new medical societies. Furthermore, community leaders and physicians perceived the dangers of crowding and poor sanitation. As a result, publications on public health began to appear, and communities were ready to be more proactive in the face of epidemic disease. It was natural that they should turn to their most trusted physicians for inoculation by the safer and less distressing Suttonian method.
The Two Doctors
Eli Todd (1769-1833) was the well-to-do son of a New Haven merchant. He was a brilliant honors graduate of Yale who had studied medicine with Dr. Ebenezer Beardsley of New Haven under the old apprentice system. He had begun practice in Farmington at the very young age of 21, and had gained the respect and love of his many patients. His were gentle treatment methods in an age of harsh remedies. His skill, kindness, and cultivation made him the favorite practitioner of the emerging wealthy class in the community. In 1792, when he joined with Theodore Wadsworth to establish the “hospital” on Rattlesnake Mountain , Todd was a hard-working 23-year-old bachelor. He had already participated in the founding of the Hartford County and Connecticut Medical societies and was active in the community, supporting the temperance movement and other worthy causes. He was an excellent musician, and a founder of the Handel Society. Membership in the local Masonic Lodge conferred status and powerful friends. In later years, he was a leading figure in the Conversation Club. The crowning achievement of Todd’s career was his role in 1819 in the founding of the Hartford Retreat for the Insane, of which he was the first director.
Todd was the younger of the two Hospital Rock doctors, but probably supplied the brain power and energy for the enterprise. He was a man of his times-the heady first years of the Republic when, under the influence of the Age of Reason, citizens were ready to take action for the betterment of society. He was also a bit of an entrepreneur: newspaper advertisements and town records show that he offered variolation at several other facilities and with various partners, last in 1801. Todd was highly altruistic, but very willing to engage in a lucrative business. Medical historian Rufus W. Mathewson commented that in 1792 “the practice of inoculation was at its height.. and a source of great income to many…. [and]the keeping of ‘pock houses’ .. was profitable.”
Todd’s partner in the enterprise was Theodore Wadsworth (1753-1808), who was slightly older, and a veteran of the Continental army. His medical training was also in the form of an apprenticeship, though we do not know his teacher’s name or whether he had attended university. In 1792 Wadsworth was 39 years old, and the father of three children. He had practiced in Southington since 1780. Nothing in the records suggests Wadsworth matched the brilliance of Todd, but he had the advantage of having practiced variolation in the army, which he joined in 1777. His military experience had no doubt taught him the highly contagious and lethal character of smallpox. Like Todd, Wadsworth had an entrepreneurial streak and participated in more than one variolation enterprise. He was also bold and original, as illustrated by the agreement (1791) documented in the Southington town records to “cure Mary Evans of her insanity for fifteen dollars . in six months. otherwise to have nothing.” Ironically, Wadsworth died in the terrible spotted fever epidemic of 1808.
The Hospital and the Rock
The hospital building stood on a stony hillside known as the “goat pasture” on Settlement Road , the old road to New Britain . The land on which the hospital was situated is believed to have belonged to the Josiah Kilbourn family, and was purchased in 1798 by Elias Brown. Both families evidently had farm buildings near the site. However it is unknown at present whether the hospital had been a farmhouse or outbuilding, or was a specially built structure. It was far from both town centers, but easily accessible for attendants and visitors with immunity. Rattlesnake Mountain sheltered the building from north winds that would otherwise chill the patients during the autumn months. Our only description of the structure comes at second hand from a patient’s grandchild, who described a long narrow building standing somewhat off the road near a spring. Inoculations were done only from about May until October, and there was no need for fireplaces.
Near the hospital building was a smooth sunny ledge on which the young patients could socialize, and where they picked up messages and packages from home. Of the hundreds who must have stayed at the hospital in the years 1792, 1793 and 1794, sixty-six have left us their names or initials cut into the ledge. It is smooth, flat and slopes down away from the old roadway. Scattered on the rock’s surface in an irregular area about 15 by 20 feet, the names are barely discernible until a visitor dusts them with flour. Then they emerge, like a photographic print materializing in a darkroom pan.
The old Settlement Road is now abandoned, though it can be traced from the quarry on Route 6 several miles through the forest to where it is interrupted by Interstate 84. Along it innumerable fragments of traprock litter the forest floor, and there area a few hints of stone walls. Near the road and 1,000 feet from the rock itself, there is a cellar hole lined with mortarless rock and a long-abandoned well. These are the only remains so far uncovered that accompany Hospital Rock with its carved names recalling a long ago and very different time.
The Patients
When news of a new smallpox epidemic came from Boston in 1792, Farmington ‘s best families entrusted their children to the charismatic Todd and to Wadsworth , his more experienced colleague
It is estimated that hundreds of patients were inoculated and spent their recovery at the Todd-Wadsworth Smallpox Hospital . Fifty-two of the 66 names carved into the rock include first, and sometimes middle, initials, and these patients can be further identified with some confidence. Considerable information is available for 26 of them. The known ages of the patients ranged from 9 to 33 years. Twelve family groups appear, and one or two parent-child pairs. The social position of the inoculees is revealing. Nineteen were descended from original proprietors of Farmington , and most appeared to come from homes of at least middling wealth. There were the children of physicians, future physicians, and future spouses of physicians. For example, the name ” Hull ” appears five times and all are descended (by various lines) from five generations of doctors. Families of clergy, judiciary, and military officers were also represented. For example, Mary Pitkin was the daughter of Timothy Pitkin, the wealthy and liberal minister of the Farmington Congregational church. Edward, Sally and William Hooker were children of Col. Noadiah Hooker who had led his troops to the smallpox-threatened siege of Boston in 1776. They were descended from Hartford founder Thomas Hooker. Names such as Cowles, Wadsworth , and Whitman abound. These youngsters were connected by blood or marriage to an extensive network of educated, wealthy and powerful Yankees.
The high cost of variolation limited the Hospital’s clientele. We do not know what Todd and Wadsworth charged for variolation, but a physician in 1764 charged the equivalent of $190 in 2001 currency, and in 1801 Todd charged a man $83 apiece (in 2001 currency) for variolating his three daughters. Free care was occasionally offered, but the uninoculated poor suffered disproportionately during epidemics.
The length of stay at the smallpox hospital varied, of course, but was generally three to four weeks. This was approximately the length of time it took for the last scab to shed. Patients were probably inoculated in small groups, to avoid the risk of cross-infection. Males and females were immunized and quarantined separately on the mountain, and while there were no scandals, lots of visiting and socializing went on. One young man stated that he was attracted to the hospital because “the girls are as thick there as toads after a rain.” There were even two marriages that took place after sojourns at Hospital Rock. One involved Dr. Wadsworth’s son, Harry, who wed Anna Mix, an inoculee, in 1807. The other marriage was of Luther Seymour and Rebekah Curtis, whose names are carved together on the rock, with the dates “1792” and “1794,” Respectively. Evidently Luther was immune, having been variolated in 1792, and had gone up to visit Rebekah in 1794 while she convalesced. They were married in Middletown in 1797, and Luther became a respected housewright, furniture maker and town librarian in Farmington .
Postscript
Variolation passed into history with the 1796 discovery by English physician Edward Jenner that infection with cowpox, a viral disease of cattle, protected milkmaids from smallpox. Cowpox, or vaccinia, virus could be passed from person to person, and resulted in immunity. Jenner’s work was quickly followed by widespread use of “vaccination” in England and after 1800 in the New World . The new procedure was much safer than variolation and just as effective. Though a few physicians continued to use variolation for a time, it was quickly supplanted. The Todd/Wadsworth hospital was no longer needed, and faded away into the woods.

Dr. Charles Leach, Farmington Town Manager Kathy Eagen, and Councilman Bill Wadsworth dusting hospital rock to facilitate reading the 200-year-old inscriptions carved in the rock. Photo courtesy of Dr. Charles Leach
There were no further significant smallpox epidemics for many years in Connecticut . Evidently because immunity waned and vaccination was neglected for a few years, an increased number of susceptibles provided the raw material for a new episode. This came in 1827, when cases in Farmington alerted the town’s officials and doctors. In response, the town undertook a thorough program of vaccination. Teams of physicians (including Todd) vaccinated hundreds of citizens at the several district schoolhouses. The epidemic was effectively stopped. The carefully-kept records of this program are now in the Farmington Room at the Town Library. Farmington again acted in response to the threat of smallpox in 1857. On a motion by Egbert Cowles Esq., it was voted that “the Selectmen be . directed to take measures to have the people of the Town vaccinated by School Districts . and use their best endeavors to have a general attendance of the People at the District School Houses to meet the Physicians..” In later years, vaccination was more routinely done, and the need for revaccination was recognized. Eventually, smallpox immunization became a requirement for admission to school and remained so until the disease was declared eradicated by the World Health Organization in 1980.
 The last small local outbreak of smallpox occurred in 1918, and was recalled by Farmington ‘s revered Dr. Edward Dunn, along with the influenza epidemic, as his “welcome to town.” The last case in the United States was recorded in 1949, and the last naturally occurring case in the world was recorded in Somalia in 1977. As the result of a massive years-long effort by the World Health Organization, smallpox became the first living species to be deliberately made “extinct” by man. (At present stocks of the virus are held in freezers at the Centers for Disease Control and in Moscow .) No vaccinations had been done since 1980 until fear of terrorism led to resumption in 2002.
The last small local outbreak of smallpox occurred in 1918, and was recalled by Farmington ‘s revered Dr. Edward Dunn, along with the influenza epidemic, as his “welcome to town.” The last case in the United States was recorded in 1949, and the last naturally occurring case in the world was recorded in Somalia in 1977. As the result of a massive years-long effort by the World Health Organization, smallpox became the first living species to be deliberately made “extinct” by man. (At present stocks of the virus are held in freezers at the Centers for Disease Control and in Moscow .) No vaccinations had been done since 1980 until fear of terrorism led to resumption in 2002.
Hospital Rock has for two centuries rested on the periphery of Farmington history. Since even local historians have been uncertain of its location, it has acquired an aura of mystery and romance. Yet it has remained a very meaningful artifact, speaking to us in a direct and moving way from the past. In the last few years, however, there has been renewed and effective interest in its preservation. While the site is actually in Farmington , the land is owned by Hartford , which purchased it for its watershed. In 2002 the Connecticut Historical Commission declared Hospital Rock and the surrounding forest to be an Historic Archeological Site, and Farmington is collaborating with Hartford in a move to gain easement protection for the site. An archeological search for the remains of the hospital itself is projected for the near future. There remains, however, the intriguing question of how to preserve the inscribed slab of bedrock out in the woods.
Dr. Charles Leach is a retired cardiologist, past president of Farmington Historical Society, and a member of the Farmington Historic District Commission.
Explore!
“Restoring East Granby’s Smallpox Cemetery,” Summer 2014 CLICK HERE TO READ
Read more stories about health history in the Feb/Mar/April 2004 and Spring 2007 issues and on our Health & Medicine TOPICS page.
Subscribe/Buy the Issue!